Epidemics have taken a toll in the Global South in recent years, re-emerging into popular discourse. Diseases such as the Ebola virus in West Africa, the plague epidemic in Madagascar, and cholera in Yemen have drastically impacted upon the lives of those affected. The World Health Organization intervenes as communicable and waterborne diseases spread across a globalizing planet, resulting in significant mortalities and causing even those fortunate enough to survive to have to adapt their personal worlds to sickness and death. These epidemics function not purely on a biological level, but are closely interconnected with society and politics on a local and global scale. Many have a history linked with global trade, imperialism, or trauma, such as war or poverty. Hidden in discourses of disease are therefore instances where people—most notably racial and religious minorities—also emerge as disease agents, victims, or both.
Death tolls, migration flow, and public health measures of North African port cities have historically been shaped by epidemics. In the nineteenth century Alexandria, Tripoli, and Tunis, which were part of Ottoman provinces subject to modernization projects and imperialism, underwent a range of commercial, political, and public health transformations. As ports, having served as entry and regulation points for goods, slaves, merchants, and migrants, they serve well as case studies—using commercial, diplomatic, and health records—through which to understand such dynamics. Epidemics entered their ports not unconnected from social context but depending on how officials negotiated trade, and based on assumptions about who would be infected.
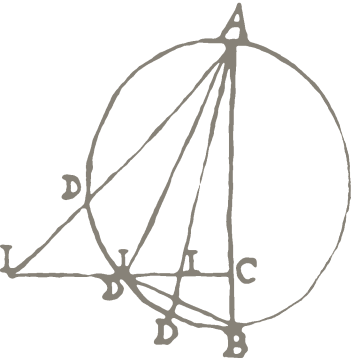
Assumptions about race were closely connected to perceptions and control of disease. During the 1850s, cholera emerged in several Mediterranean ports, commonly reported by European merchants and locals who cited ships and their goods as victims of disease. The British consul in Tunis surmised that 415 pilgrims were possible carriers of the 1850 cholera epidemic. It was also inferred that this same ship passing through Tunis reached Tripoli, thus leading to another outbreak, “hitherto it has chiefly been fatal to Jews and a few Maltese.” Cholera wasn’t the only concern when it came to disease: on 11 September 1850, a Sir … Crowner stated that “109 Christians, 39 Jews, and 67 Turks and Moors” died from the plague (Fig. 1).
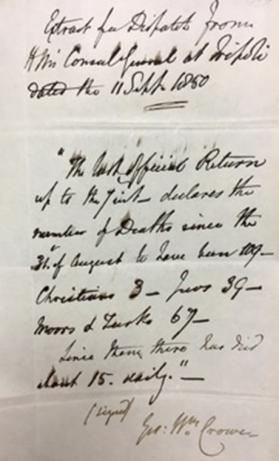
Fig. 1: Statement on plague deaths in Tripoli, 1850. Source: British National Archives, 11. BNA MH 13/254, Folio 301, Tripoli, 21, September 1850.
The port of Tripoli was connected with Alexandria, Marseilles, and Tunis, and like several North African port cities, experienced trade and plague. What makes this report unique is the racial marking of non-Christians: the indigenous people of Tripoli were marked as Moor—rather than Arab, Amazigh, Black, or Muslim—and the Jewish population was tallied separately from the Moors/Turkish group.
Disease also impacted upon the way in which health was regulated on a global scale. Modernization and reform projects led to calls for sanitation, part of the internationalization of health regulation and an attempt to create semi-autonomous rule. Quarantine became a central element in the way in which international bodies regulated goods and people. Article 124 of the Paris International Sanitary Convention (1852), which stipulated how ports should monitor disease, resulted in the Alexandria (Egypt) Board of Health being made independent of the local government, thus positioning health under international governance. Networks such as the International Sanitary Conference (which preceded the formation of the World Health organization in 1948), and extra-governmental public health bodies such as the Alexandria Quarantine Board were established to manage and regulate disease. This global–level regulation was not restricted to Alexandria: in 1886 the Tunis newspaper Ra’id al-tunisi printed international quarantining regulations, binding Tunisian people to the protocol of the masses.
Fig. 2: Gulf of Tunis. Source: The Hebrew University of Jerusalem.
Health institutions and regulations such as those mentioned above were commonly established as a result of the epidemics associated with travel and trade. Yet the expediency of trade appeared to matter more than containing disease. On 27 July 1885, the President to the Egyptian Maritime and Quarantine Board of Health Walter F. Miéville claimed:
“As regards England, also, there is a special reason why ships bound to her own ports should not be bound by rules which the Mediterranean Powers may think necessary, since the time occupied in sailing from Egypt to ports in the United Kingdom is itself a sufficient quarantine.”
This particular junction highlights how profit can sometimes overturn health regulations, on a global as well as local scale.

Fig. 3: Port of Tunis, Entrance by the S.A. Ryale from the Port of La Goulette. Source: Bibliothèque nationale de France.
Into the twentieth century, Alexandria, Tripoli, and Tunis also featured into geopolitical conceptions of disease during World War I, which found itself on the shores of North Africa. The Senussi Campaigns (1915–17) operated within a European theatre, but also came with broader measures to influence public health. Sanitation was tied to military medicine, and the health of troops formed part of the military operation. By 1919, the British Foreign Office used prophylactic measures to prevent the spread of infectious diseases into Europe. This was part of the post-World War I British proposal for a railway and pipeline from the Mosul area to Tripoli. The power to define infectious encounters became crucial and contentious for a wide range of actors, but also came with public health institutions and regulations that curtailed certain goods and groups of people from traveling through.
Epidemics are not merely biological agents that travel through vectors such as clothing or people: they exert a broader influence corresponding with anthropogenic, geopolitical, and material forces. As part of Department III’s research theme “Histories of Planning,” this research will incorporate and problematize such influences on public health and scientific practice in the context of epidemics in North Africa and the Middle East, connecting them to present-day issues.